
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- The Association between Pulmonary Functions and Incident Diabetes: Longitudinal Analysis from the Ansung Cohort in Korea (Diabetes Metab J 2020;44: 699-710)
- Hoon Sung Choi, Sung Woo Lee, Jin Taek Kim, Hong Kyu Lee
- Diabetes Metab J. 2020;44(6):944-945. Published online December 23, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0249
- 3,457 View
- 61 Download
- Metabolic Risk/Epidemiology
- The Association between Pulmonary Functions and Incident Diabetes: Longitudinal Analysis from the Ansung Cohort in Korea
- Hoon Sung Choi, Sung Woo Lee, Jin Taek Kim, Hong Kyu Lee
- Diabetes Metab J. 2020;44(5):699-710. Published online April 16, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0109
- 6,170 View
- 104 Download
- 9 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background We sought to explore whether reduced pulmonary function is an independent risk factor for incident diabetes in Koreans.
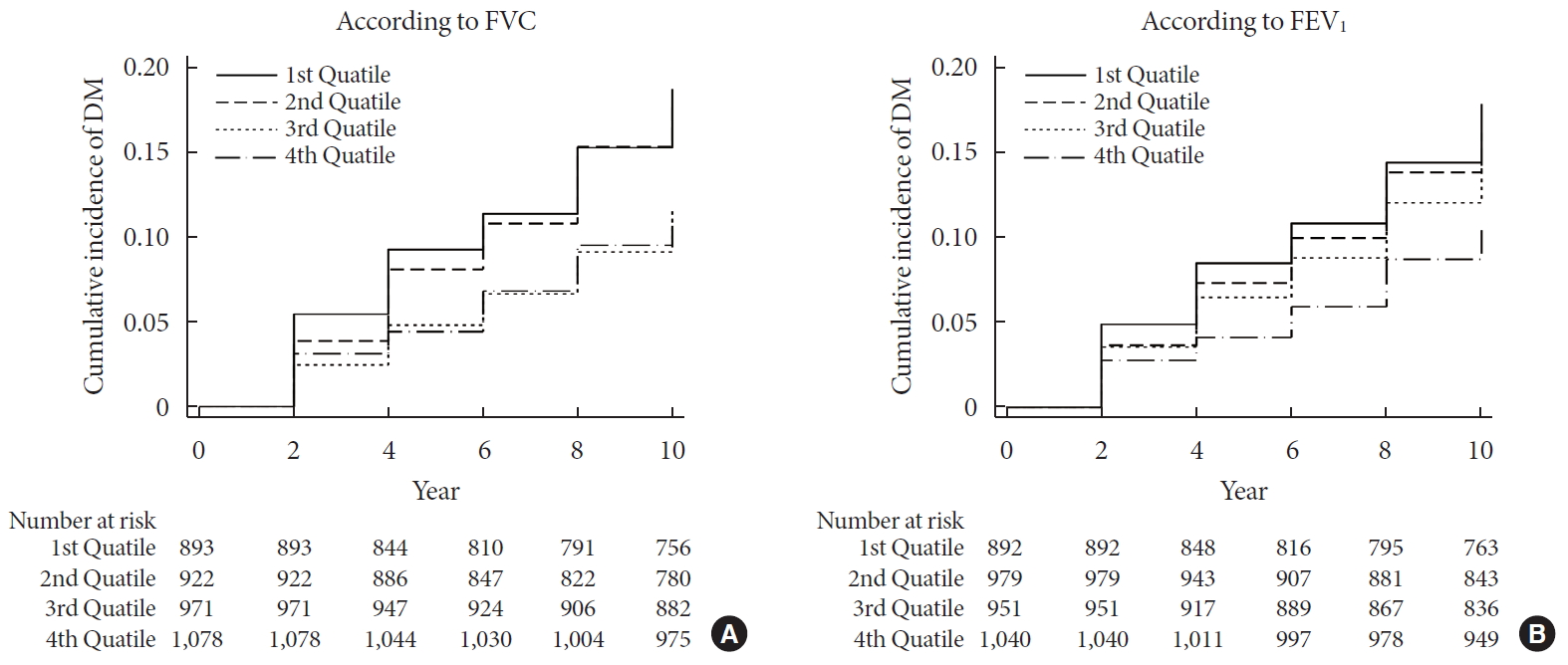
Methods We conducted a prospective cohort study of pulmonary function as a risk factor for incident diabetes using 10-year follow-up data from 3,864 middle-aged adults from the Ansung cohort study in Korea. The incidence of diabetes was assessed using both oral glucose tolerance tests and glycosylated hemoglobin levels.
Results During 37,118 person-years of follow-up, 583 participants developed diabetes (incidence rate: 15.7 per 1,000 person-years). The mean follow-up period was 8.0±3.7 years. Forced vital capacity (FVC; % predicted) and forced expiratory volume in 1 second (FEV1; % predicted) were significantly correlated with incident diabetes in a graded manner after adjustment for sex, age, smoking, exercise, and metabolic parameters. The adjusted hazard ratio (HR) and confidence interval (CI) for diabetes were 1.408 (1.106 to 1.792) and 1.469 (1.137 to 1.897) in the first quartiles of FVC and FEV1, respectively, when compared with the highest quartile. Furthermore, the FVC of the lowest first and second quartiles showed a significantly higher 10-year panel homeostasis model assessment of insulin resistance index, with differences of 0.095 (95% CI, 0.010 to 0.018;
P =0.028) and 0.127 (95% CI, 0.044 to 0.210;P =0.003), respectively, when compared to the highest quartiles.Conclusion FVC and FEV1 are independent risk factors for developing diabetes in Koreans. Pulmonary factors are possible risk factors for insulin resistance and diabetes.
-
Citations
Citations to this article as recorded by- Validation of the Framingham Diabetes Risk Model Using Community-Based KoGES Data
Hye Ah Lee, Hyesook Park, Young Sun Hong
Journal of Korean Medical Science.2024;[Epub] CrossRef - Independent and combined associations of multiple-heavy-metal exposure with lung function: a population-based study in US children
Yiting Chen, Anda Zhao, Rong Li, Wenhui Kang, Jinhong Wu, Yong Yin, Shilu Tong, Shenghui Li, Jianyu Chen
Environmental Geochemistry and Health.2023; 45(7): 5213. CrossRef - Role of Pulmonary Function in Predicting New-Onset Cardiometabolic Diseases and Cardiometabolic Multimorbidity
Guochen Li, Yanqiang Lu, Yanan Qiao, Die Hu, Chaofu Ke
Chest.2022; 162(2): 421. CrossRef - Reduced lung function predicts risk of incident type 2 diabetes: insights from a meta-analysis of prospective studies
Yunping Zhou, Fei Meng, Min Wang, Linlin Li, Pengli Yu, Yunxia Jiang
Endocrine Journal.2022; 69(3): 299. CrossRef - Development of Various Diabetes Prediction Models Using Machine Learning Techniques
Juyoung Shin, Jaewon Kim, Chanjung Lee, Joon Young Yoon, Seyeon Kim, Seungjae Song, Hun-Sung Kim
Diabetes & Metabolism Journal.2022; 46(4): 650. CrossRef - Improving Machine Learning Diabetes Prediction Models for the Utmost Clinical Effectiveness
Juyoung Shin, Joonyub Lee, Taehoon Ko, Kanghyuck Lee, Yera Choi, Hun-Sung Kim
Journal of Personalized Medicine.2022; 12(11): 1899. CrossRef - The Association between Pulmonary Functions and Incident Diabetes: Longitudinal Analysis from the Ansung Cohort in Korea (Diabetes Metab J 2020;44: 699-710)
Hoon Sung Choi, Sung Woo Lee, Jin Taek Kim, Hong Kyu Lee
Diabetes & Metabolism Journal.2020; 44(6): 944. CrossRef - The Association between Pulmonary Functions and Incident Diabetes: Longitudinal Analysis from the Ansung Cohort in Korea (Diabetes Metab J 2020;44: 699-710)
Jin Hwa Kim
Diabetes & Metabolism Journal.2020; 44(6): 940. CrossRef
- Validation of the Framingham Diabetes Risk Model Using Community-Based KoGES Data
- Prevalence and Clinical Characteristics of Aspirin Resistance in the Patients with Type 2 Diabetes Mellitus.
- Mi Yeon Kang, Young Min Cho, Hyun Kyung Kim, Jee Hyun An, Hwa Young Ahn, Ji Won Yoon, Hoon Sung Choi, Jie Seon Lee, Kyong Soo Park, Seong Yeon Kim, Hong Kyu Lee
- Korean Diabetes J. 2008;32(1):53-59. Published online February 1, 2008
- DOI: https://doi.org/10.4093/kdj.2008.32.1.53
- 2,500 View
- 22 Download
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
We examined the prevalence and clinical characteristics of aspirin resistance in the Korean patients with type 2 diabetes mellitus. METHODS: We studied 181 Korean patients with type 2 diabetes mellitus who were taking aspirin (100 mg/day for > or = 3 months) and no other antiplatelet agents. The VerifyNow System was used to determine aspirin responsiveness. Aspirin resistance was defined as an aspirin reaction unit (ARU) > or = 550. We measured the cardio-ankle vascular index (CAVI) and ankle-brachial index (ABI) to evaluate arteriosclerosis. The anthropometric parameters, electrocardiogram, blood pressure, fasting plasma glucose, lipid profiles, hemoglobin A1c, highly sensitive C-reactive protein (hsCRP), homocysteine, and microalbuminuria were measured in each patient. RESULTS: The prevalence of aspirin resistance in type 2 diabetic patients was 9.4% (17 of 181). Those who had aspirin resistance were older than those without aspirin resistance (64.6 +/- 10.6 vs. 59.8 +/- 8.1, P = 0.024). Aspirin resistance was not associated with fasting plasma glucose, total cholesterol, triglyceride, LDL-cholesterol, HDL-cholesterol, hemoglobin A1c, hsCRP, homocysteine, microalbuminuria, ABI, CAVI, and body mass index. CONCLUSION: Prevalence of aspirin resistance in the Korean patients with type 2 diabetes mellitus was 9.4%. Although aspirin resistance was associated with old age, we could not find any good clinical parameter to predict it. Therefore, aspirin resistance should be evaluated in diabetic patients taking aspirin for prevention of cardiovascular complications. -
Citations
Citations to this article as recorded by- Long Non-Coding RNA H19 Positively Associates With Aspirin Resistance in the Patients of Cerebral Ischemic Stroke
Jue Wang, Bin Cao, Yan Gao, Dong Han, Haiping Zhao, Yuhua Chen, Yumin Luo, Juan Feng, Yanxia Guo
Frontiers in Pharmacology.2020;[Epub] CrossRef - 6th Asian PAD Workshop
Annals of Vascular Diseases.2015; 8(2): 135. CrossRef - Non-HDL cholesterol is an independent risk factor for aspirin resistance in obese patients with type 2 diabetes
Jong Dai Kim, Cheol-Young Park, Kue Jeong Ahn, Jae Hyoung Cho, Kyung Mook Choi, Jun Goo Kang, Jae Hyeon Kim, Ki Young Lee, Byung Wan Lee, Ji Oh Mok, Min Kyong Moon, Joong Yeol Park, Sung Woo Park
Atherosclerosis.2014; 234(1): 146. CrossRef
- Long Non-Coding RNA H19 Positively Associates With Aspirin Resistance in the Patients of Cerebral Ischemic Stroke

 KDA
KDA
 First
First Prev
Prev





